The 4th Trimester and Beyond
By Alexis Eusterbrock, DPT, COMT, OCSBy Alexis Eusterbrock, DPT, COMT, OCS
I started to brainstorm and write this blog nearly a year ago after returning to work following maternity leave with my second child. My motivation for writing this blog is to bring greater awareness to the importance of true REHABILITION following childbirth. Currently there is pressure in our society to return to your previous life and body as soon as possible following birth. Women are not given the same time and resources to heal, recover, and truly rehabilitate following childbirth as we give following other injuries or procedures. It is common practice to expect a nine to twelve-month recovery period with a guided rehabilitation program after most orthopedic surgeries. Following childbirth, women are most often cleared to return to normal activities 6-8 weeks following delivery with little to no guidance on how to do so effectively to promote physical recovery, tissue healing, efficient functional mechanics, proper muscle control, and emotional well-being. Some recent improvements have been made to postpartum care, but I believe we can do better.
The 4th trimester?
The 4th trimester is defined as the first three months of your baby’s life, historically focused around the care of the newborn, with more recent focus on improving care of the mother in this period. However, the two are very intertwined as it has been shown that maternal health is directly tied to the health of infants and children. To increase the focus on maternal care, in May 2018, the American College of Obstetricians and Gynecologists (ACOG) came up with new care recommendations in the postpartum period which include a check in with your obstetric care provider in the first 3 weeks postpartum. Ongoing care is to be provided on an individualized basis with a comprehensive postpartum visit no later than 12 weeks postpartum. A primary provider for this postpartum care should be identified to help to facilitate referrals to a team of care providers including pelvic health physical therapists, psychotherapists, lactation consultants, etc, to address “mood and emotional well-being; infant care and feeding; sexuality, contraception, and birth spacing; sleep and fatigue; physical recovery from birth; chronic disease management; health maintenance.” Many, including myself, would argue that this period of postpartum recovery extends beyond this first three months and into the entire year postpartum and beyond for some women.
The postpartum period is also a time of great physiological and psychosocial change for new moms. Stress levels can be high as you work to meet the demands of caring for your new baby (and potentially other family members), and there is less time for your own self-care. Clinical postpartum depression is reported to occur in 10% of women; with rates varying by state, by age, and by race/ethnicity. And postpartum anxiety disorders have been reported to have an incidence of 6.1%-27.9%. When postpartum anxiety and/or depression is present, it can further distance a mother from being able to provide time for the self-care and recovery she needs.
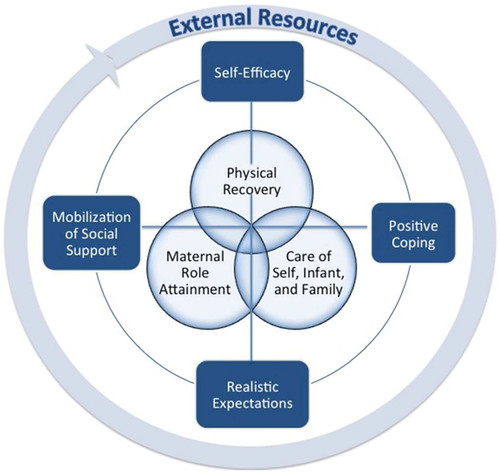
In this vein, a more comprehensive perinatal health promotion model (see image below) was presented by Fahey in 2013 to better encompass the biopsychosocial aspects of maternal care.
This model and ACOG’s recent change to postpartum care recommendations is encouraging, but, it is still evident that we need better and more comprehensive care for women postpartum. Education and awareness needs to improve so women do not have to rely only on their health care providers for referrals, but can also be advocates for their own care.
Physical recovery from birth is where pelvic health physical therapists and/or orthopedic physical therapists can be of great help! There are a number of symptoms that women may experience postpartum including:
- Urinary incontinence
- Fecal incontinence
- Gas incontinence
- Pelvic pain
- Pain with sexual activity
- Pelvic organ prolapse symptoms
- Back pain
- Hip pain
- Sacral and/or tailbone pain
- Pain or discomfort at a c-section scar
- Constipation
- Abdominal pain and/or weakness
- Aches and pains with physical stresses of caring for a newborn and/or other young children
These all can be normal symptoms!! And it is OK to seek care for these concerns! I can’t tell you the number of times I hear the phrase from my patients, “why has no one mentioned this before,” in response to pelvic health issues. And a sense of frustration that they have never been told there was an alternative to “just dealing with symptoms.” Many of the symptoms above are related to pelvic floor dysfunction and can be improved with care.
In closing, my hope for anyone reading this blog is to join me and many other women’s healthcare providers on the soap box of expecting better, more comprehensive care for women in the postpartum period. However long that might be for each woman. And it is individual, recovery may take months for some and years for others. Please reach out if our team at Stride can help in your postpartum journey!
References
- American College of Obstetrics and Gynecology (Acog.org)
- Kathe Wallace Pelvic Resources (Kathewallace.com)
- Centers for Disease Control (Cdc.gov)
- Fahey, J and Shenassa, E Understanding and Meeting the Needs of Women in the Postpartum Period: The Perinatal Maternal Health Promotion Model. Journal of midwifery and women’s health. 12/2013.
- Ali, E Women’s experience with postpartum anxiety disorders: a narrative literature review. International Journal of Women’s Health. 2018; 10: 237-249.
- Image credit: https://depositphotos.com/113334862/stock-illustration-set-silhouette-sketch-mother-and.html